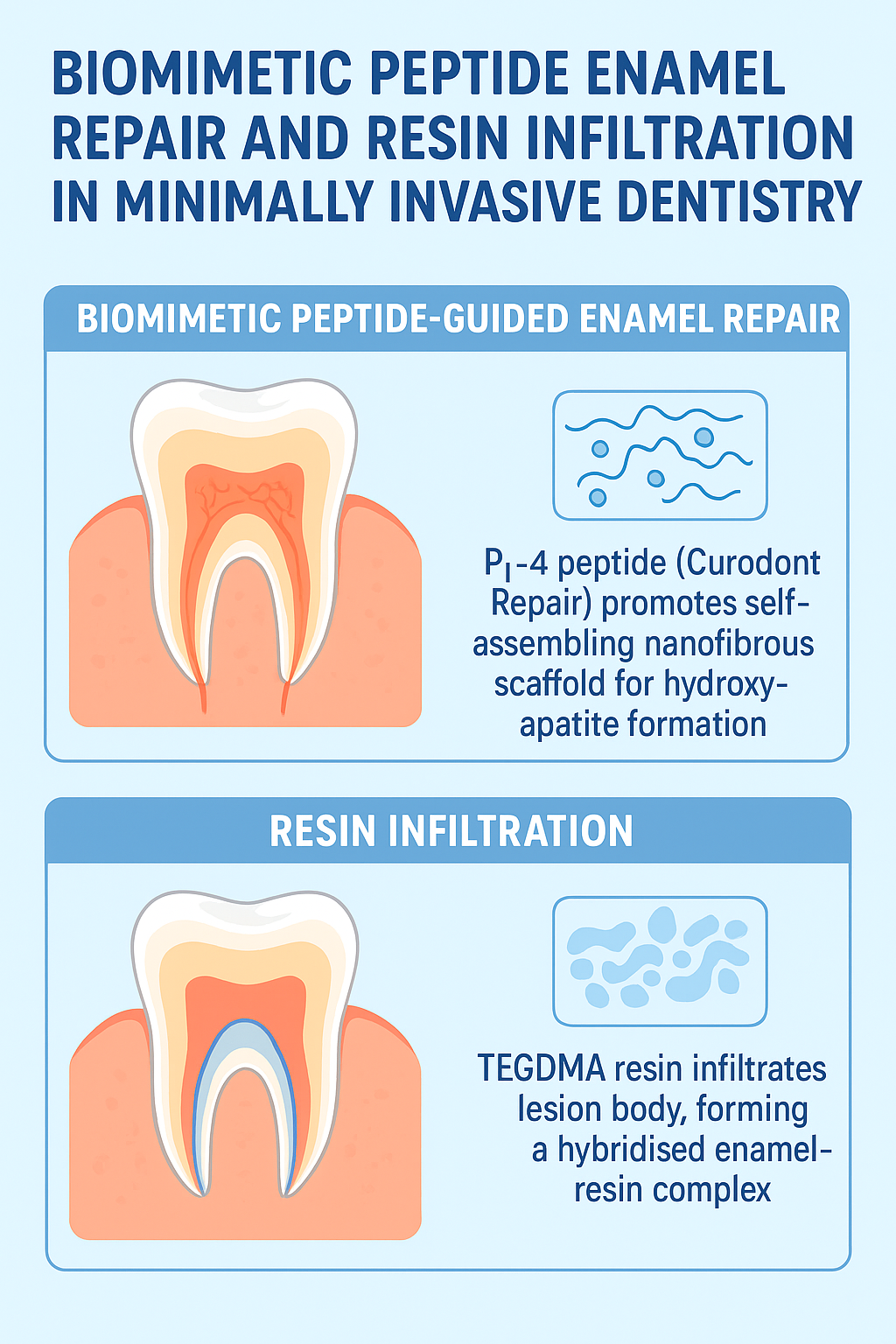
- ICDAS 1 (early enamel change when air-dried): Peptide-guided regeneration is preferred.
- ICDAS 2 (visible enamel change when wet) with aesthetic concerns: Resin infiltration, alone or combined with peptide therapy.
About the Author
Dr. Hajeera Banu is a skilled dentist who graduated from RGUHS in 2014 and has since built a successful career in the field. With a strong focus on implants, restorative dentistry, and aligners, she has honed her expertise to offer her patients the highest level of care. Based in Mysore, India, Dr. Banu runs her own private practice, where she combines advanced dental techniques with a patient-centered approach.
Her passion for dentistry extends beyond her practice; she stays up-to-date with the latest advancements in the field to ensure she delivers the best outcomes. Outside of her professional life, Dr. Banu enjoys blogging, where she shares insights and experiences from her dental journey, as well as her love for cooking and traveling. These interests help to balance her dynamic lifestyle, and she continues to seek personal and professional growth in all aspects of her life. email dentistryunited@gmail.com