Occlusal splints are among the most versatile tools in dentistry. For decades, they have been prescribed to protect teeth from nocturnal bruxism, relieve jaw muscle fatigue, and stabilize occlusion. Yet, in the context of Neuromuscular Dentistry (NMD), their role extends far beyond protection. Splints become diagnostic instruments, therapeutic mediators, and platforms for long-term rehabilitation.
When appropriately designed and applied, functional occlusal splints help patients transition from dysfunction to stability—relieving pain, correcting mandibular posture, and restoring harmony between teeth, muscles, and joints.
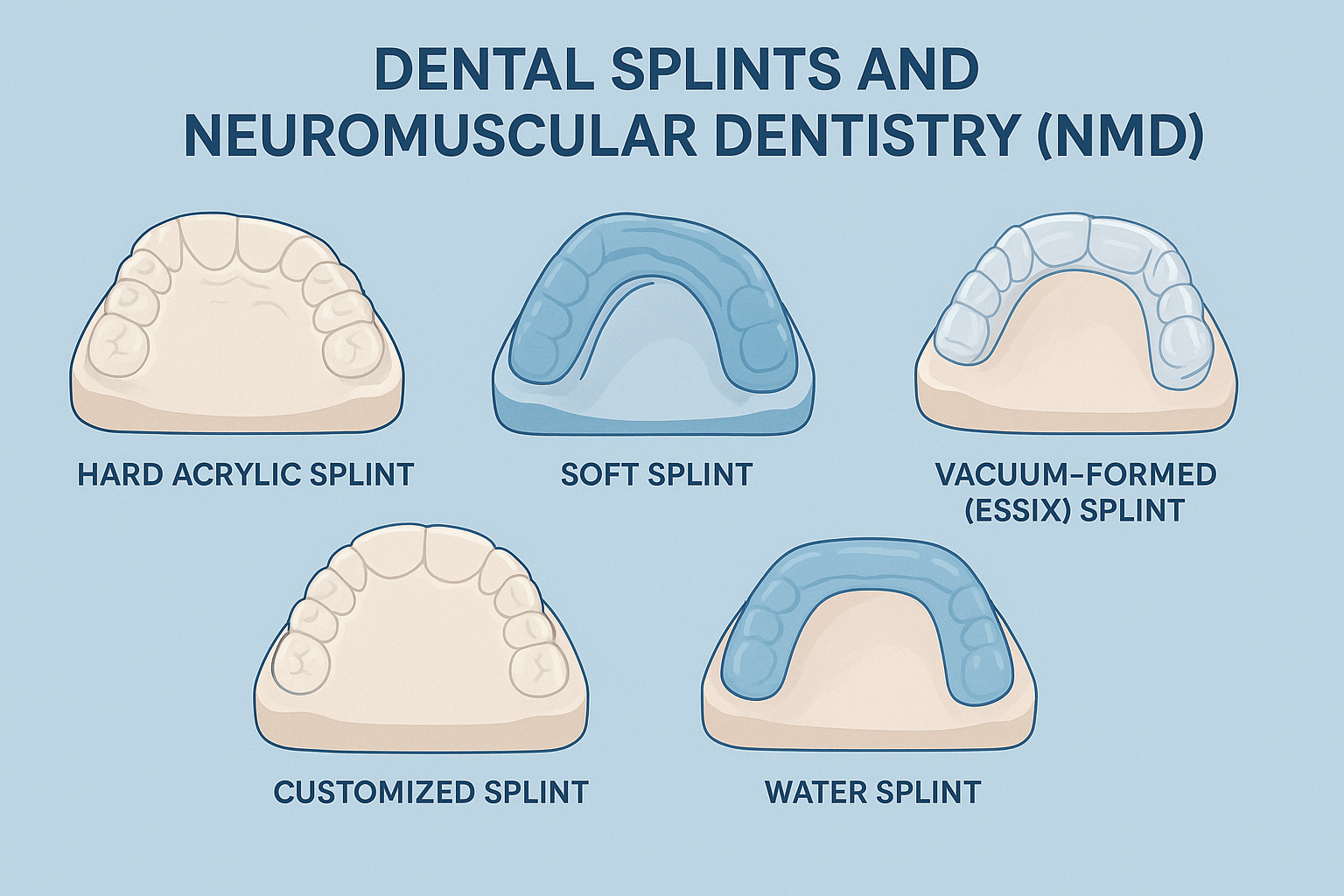
Classification of Functional Occlusal Splints
Not all splints are created equal. Their form and function depend on clinical objectives, patient condition, and biomechanical philosophy.
1. Stabilization Splints (Permissive Splints)
- Purpose: Permit the mandible to settle into a musculoskeletally stable position.
- Mechanism: Create broad, even contacts across the arch, reducing hyperactivity of elevator muscles and protecting the dentition.
- Indications: Bruxism, diffuse muscle pain, and generalized occlusal instability.
2. Repositioning Splints (Directive Splints)
- Purpose: Direct the mandible into a new therapeutic position.
- Mechanism: Often advance the mandible to recapture a displaced disc or relieve a compressed condyle.
- Indications: Disc displacement with reduction (clicking joints), chronic condylar compression, or cases requiring joint unloading.
3. Deflective/Hybrid Splints
- Purpose: Combine permissive and directive features.
- Example: An anterior bite plane deprogrammer that disengages posterior teeth while influencing mandibular posture.
- Indications: Muscle deprogramming and diagnostic evaluation.
4. Water Splints (Hydrostatic Splints)
- Design: Fluid-filled pads (Aqualizer® type).
- Mechanism: Provide a hydrostatic balance that dynamically equalizes occlusal forces.
- Indications: Acute TMD pain, rapid deprogramming, and interim relief.
- NMD Relevance: Ideal for muscle relaxation prior to recording a neuromuscular bite.
5. Customized Digital Splints (CAD-CAM)
- Design: Fabricated via intraoral scanning and 3D milling/printing.
- Advantages: Precision fit, durability, comfort, and adaptability to specific therapeutic positions.
- NMD Relevance: Maintain EMG- and TENS-determined mandibular posture; integrate with digital occlusal analysis such as T-Scan.
6. Essix Splints (Vacuum-Formed Appliances)
- Design: Thin thermoplastic devices, similar to retainers.
- Advantages: Transparent, lightweight, and aesthetic.
- Limitations: Less durable; not suited for heavy bruxers or major repositioning.
- Indications: Mild bruxism, post-orthodontic interim use, or transitional protection.
Indications for Occlusal Splints
- Bruxism and clenching: Preventing wear, fractures, and restoration failures.
- TMD symptoms: Clicking, locking, joint pain, or myofascial tenderness.
- Occlusal/postural imbalance: Restoring mandibular equilibrium.
- Adjunctive therapy: Supporting orthodontic or prosthodontic planning.
- Diagnostic tool: Testing therapeutic positions before definitive rehabilitation.
Clinical Procedure
- Impression and Bite Registration
- Preliminary alginate or digital scan; final PVS or VPS impressions.
- Bite taken in centric relation (stabilization splints) or guided therapeutic position (repositioning splints).
- Laboratory Fabrication
- Acrylic resin or CAD-CAM milling.
- Mounted on an articulator using facebow transfer where needed.
- Insertion and Adjustment
- Ensure bilateral, simultaneous contacts.
- Establish smooth anterior or canine guidance.
- Follow-Up and Maintenance
- First review at 1–2 weeks; then at 4–6 week intervals.
- Adjustments as symptoms resolve and occlusion adapts.
Clinical Vignettes
Case 1: Acute Clicking TMJ Managed with Water Splint
A 32-year-old IT professional presented with right-sided TMJ clicking and morning stiffness. Examination revealed disc displacement with reduction and masseter tenderness.
- Phase 1: A hydrostatic water splint was provided. Within 72 hours, joint noise diminished, and muscle tightness eased.
- Phase 2: Using low-frequency TENS and electromyography, a neuromuscular bite was recorded.
- Phase 3: A CAD-CAM stabilization splint was fabricated in this therapeutic position. Clicking resolved, and the patient entered long-term monitoring.
Key Point: Water splints provide immediate deprogramming, but definitive stabilization requires a customized neuromuscularly guided appliance.
Case 2: Bruxism and Wear Managed with Customized Splint
A 47-year-old teacher presented with attrition, abfractions, and fractured composites. Her spouse reported nocturnal grinding.
- Phase 1: An Essix splint was prescribed for short-term protection.
- Phase 2: A CAD-CAM hard acrylic stabilization splint was fabricated from digital scans and adjusted with T-Scan analysis.
- Phase 3: EMG confirmed reduced elevator muscle activity after 4 weeks, and restorative rehabilitation was initiated.
Key Point: Essix appliances serve as useful interim protectors, but long-term neuromuscular stability requires customized splints.
Neuromuscular Dentistry Perspective
Splints embody the philosophy of NMD, which seeks harmony between teeth, muscles, and joints:
- Muscle Deprogramming: Removing occlusal interferences allows muscles to relax into true physiologic rest.
- EMG and TENS Guidance: Splints preserve the ideal mandibular posture established by objective neuromuscular recordings.
- Joint Stabilization: Repositioning splints can recapture displaced discs and unload joints.
- Platform for Rehabilitation: The therapeutic bite established via splints becomes the foundation for orthodontic, prosthodontic, or restorative care.
Role in TMD Clicking and Long-Term Care
- Clicking joints: Repositioning splints stabilize or recapture disc-condyle relationships.
- Pain relief: Splints redistribute occlusal load, reducing muscle and ligament strain.
- Initiating treatment: Splints are often the first step before definitive NMD-guided rehabilitation.
- Preventing relapse: Long-term stabilization prevents recurrence of joint dysfunction.
Precautions and Clinical Considerations
- Compliance: Regular wear is essential for therapeutic success.
- Monitoring: Unsupervised long-term use, especially of repositioning splints, risks permanent occlusal change.
- Hygiene: Daily cleaning is mandatory to avoid plaque and fungal buildup.
- Customization: Not all TMD cases require splints; accurate diagnosis is critical.
- Adjunctive role: Physiotherapy, postural correction, and behavioral interventions often enhance splint therapy outcomes.
Conclusion
Functional occlusal splints are no longer passive protectors; they are active mediators of health and stability. From water-based hydrostatic devices for immediate relief to digitally customized splints for long-term neuromuscular stabilization, they represent both the art and science of modern dentistry.
When guided by NMD principles, splints reduce pain, eliminate clicks, stabilize joints, and pave the way for definitive rehabilitation. They are not an endpoint but a gateway—leading patients from dysfunction toward equilibrium, from chronic discomfort to restored physiologic balance.

Author: Dr. Syed Nabeel, BDS, D.Orth, MFD RCS (Ireland), MFDS RCPS (Glasgow), is a clinician-scholar whose career spans over two decades at the intersection of orthodontics, neuromuscular dentistry, and digitally integrated diagnostics. As Clinical Director of Smile Maker Clinics Pvt. Ltd., he has pioneered a philosophy of care rooted in anatomical precision, occlusal neurophysiology, and contemporary AI-enhanced workflows. A Diplomate in Orthodontics from Italy and an alumnus of advanced programs at Various International Universiteis , Dr. Nabeel brings a globally benchmarked clinical acumen to the nuanced management of temporomandibular disorders, esthetic rehabilitation, and algorithm-guided orthodontics.
In 2004, he founded DentistryUnited.com, a visionary platform connecting over 40,000 dental professionals through peer learning and collaborative dialogue. His academic drive led to the launch of Dental Follicle – The E-Journal of Dentistry (ISSN 2230-9489), a peer-reviewed initiative now indexed in EBSCO, fostering interdisciplinary scholarship across clinical domains.
A prolific educator, he has contributed to UGC and national broadcast media as a subject expert and regularly speaks at scientific forums, favoring small-group, discussion-based formats that emphasize clinical realism over theoretical abstraction. His ethos remains steadfast: knowledge, when shared freely, multiplies in value. Dr. Nabeel continues to shape the future of dentistry through research, mentorship, and his enduring commitment to elevating practice standards in India and beyond.