When Abutments Diverge: Navigating the Challenges of Unparallel Teeth in Fixed Partial Dentures
In the intricate world of restorative dentistry, the quest for prosthetic harmony often hinges on a fundamental principle: parallelism of abutment teeth. As an alumnus of the Royal College of Surgeons in Ireland, where I honed my skills in prosthodontics amid a rigorous curriculum blending anatomy, biomechanics, and patient-centered care, I’ve witnessed how seemingly subtle misalignments can unravel even the most meticulously planned fixed partial dentures—commonly known as bridges. For clinicians worldwide, from bustling urban practices in Dublin to remote clinics in Southeast Asia, managing unparallel abutments demands not just technical prowess but a deep appreciation of occlusal dynamics and long-term oral health implications. This article delves into the science, strategies, and evolving solutions for these cases, emphasizing how tilted teeth can precipitate temporomandibular disorders (TMD) and complicate occlusal restoration, while underscoring bridges’ enduring role despite the implant era. With digital dentistry advancements accelerating in 2025, we also explore why integrating tools like CAD/CAM and AI is imperative for crowns and bridges, alongside the growing necessity of orthodontic interventions—such as braces or Invisalign—for achieving abutment parallelism.
The Biomechanical Imperative of Parallelism
At its core, a bridge’s success rests on a unified path of insertion, where abutments align to permit seamless seating of the prosthesis. Divergent angles disrupt this, leading to incomplete fit, undue stress on supporting structures, and accelerated wear. Clinically, this manifests as uneven force distribution: tilted abutments channel occlusal loads laterally, inducing shear forces that compromise cement integrity and abutment vitality. In my experience, ignoring these discrepancies has led to debonding or fracture rates climbing as high as 20% within five years, a stark reminder of why early detection—via diagnostic wax-ups or digital scans—is paramount.
Etiologies of Divergence
Unparallelism often stems from physiological drifts, such as post-extraction tilting of molars, aberrant eruption paths in mandibular second molars, or iatrogenic factors like inconsistent preparation angles. Globally, these issues transcend demographics; in regions with high edentulism rates, such as parts of Europe and Asia, drifted teeth exacerbate the challenge, turning routine restorations into complex interventions.
Occlusal Ramifications: From Tilted Teeth to TMD and Beyond
Severely inclined abutments extend their mischief beyond the prosthesis, perturbing the delicate equilibrium of occlusion and potentially igniting temporomandibular disorders. Tilted teeth alter mandibular kinematics, forcing compensatory muscle activations—think masseter and temporalis hyperactivity—to maintain bite contact. This asymmetry overloads the temporomandibular joint (TMJ), fostering disc displacement, inflammation, and symptoms like chronic orofacial pain, headaches, and limited jaw excursion. Research highlights how malocclusion from misalignment correlates with TMD prevalence, with uneven occlusal contacts amplifying joint stresses by up to 50% during mastication. In practice, I’ve seen patients—often middle-aged with histories of tooth loss—present with TMD flares traced back to untreated tilts, where the jaw’s “locked” excursions mimic a misaligned hinge, eroding quality of life.
Compounding this, edentulous spaces invite overeruption of opposing dentition. Consider a missing lower molar: the unopposed upper tooth migrates downward, encroaching on prosthetic space and “locking” the occlusion—preventing proper bridge seating and perpetuating TMD cycles through premature contacts. Restoring harmony here requires targeted interventions. Orthodontic intrusion, using temporary anchorage devices (TADs), can retract the overerupted tooth by 2–3 mm, preserving vitality but demanding patient compliance and specialist input. For more pronounced cases (>1.5 mm supraeruption), intentional root canal therapy (RCT) emerges as a strategic pivot: devitalizing the tooth enables post-core buildup and crown placement, effectively “shortening” it to reclaim interocclusal clearance without excessive bone removal. Often paired with crown lengthening, this approach—viable for posterior teeth—restores vertical dimension, redistributes forces evenly, and mitigates TMD by realigning the occlusal plane. Long-term follow-ups affirm survival rates exceeding 90% when executed judiciously, though ethical considerations, like pulp health trade-offs, necessitate informed consent. Humanizing these decisions, I recall a patient whose debilitating jaw pain resolved post-RCT and restorative crown, transforming daily meals from agony to normalcy.
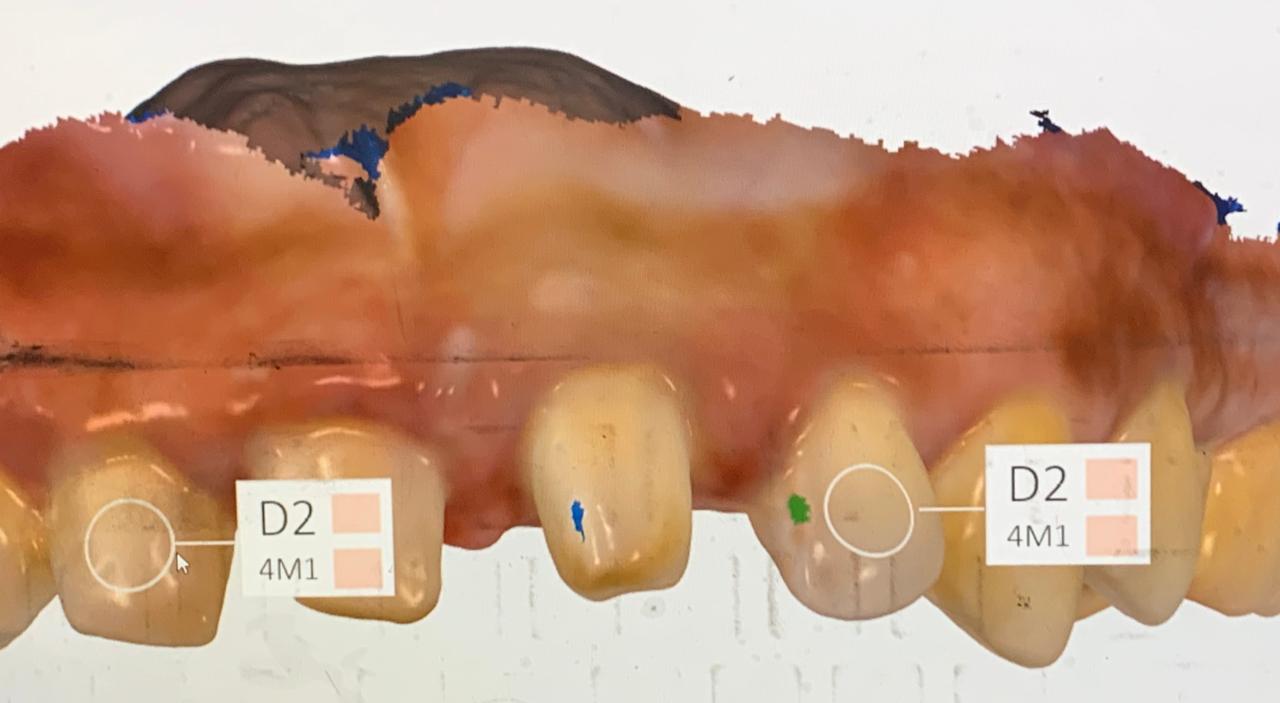
The Digital Revolution in Crowns and Bridges: Advocating for Broader Adoption
As we navigate unparallel abutments, digital dentistry stands as a transformative ally, yet its underutilization in crowns and bridges—despite proven benefits—calls for urgent wider integration in global practices. In 2025, advancements like AI-driven design and 3D printing are reshaping workflows, with 18% of U.S. dental professionals already adopting AI and 66% considering it, while intraoral scanners reach 57% penetration. CAD/CAM systems enable same-day crowns, reducing patient visits and enhancing precision by simulating insertion paths virtually, minimizing errors in parallelism. 3D printing, now in 15% of U.S. practices, accelerates temporary and even permanent restorations, with AI automating designs for bridges to compensate for divergences. Benefits abound: faster production, superior fit, and patient comfort, yet adoption lags in resource-limited settings. Embracing these tools not only streamlines abutment prep but elevates outcomes, urging clinicians to invest in training for this digital shift.
Contemporary Strategies for Correction
Balancing tissue conservation with functionality, clinicians draw from a toolkit refined by digital innovation and time-tested mechanics.
- Refinements in Tooth Modification: Subtle enameloplasty or axial recontouring addresses minor tilts, while retention slots enhance grip without over-reduction.
- Telescopic Systems: Double-crown designs—inner copings cemented to abutments, outer frameworks telescoping over them—accommodate divergence up to 20–30 degrees, distributing stresses via micro-mobility and bolstering retention in multi-abutment spans.
- Intentional Endodontics for Alignment: As noted, elective RCT facilitates aggressive preparation to enforce parallelism, particularly when vital preservation falters.
- Non-Rigid and Surveyed Adaptations: Keyway connectors act as stress directors in extended bridges, while surveyed crowns reshape contours for convergence.
- Orthodontic Interventions for Abutment Straightening: Pre-prosthetic orthodontics, including traditional braces or clear aligners like Invisalign, uprights tilted abutments to achieve parallelism, optimizing pontic space and reducing prep invasiveness. Concepts like Prosthetically Guided Orthodontics (PGO) leverage digital planning for targeted movements, enhancing bridge fit and aesthetics in 4–14 weeks. Invisalign, adaptable even with existing crowns, aligns teeth pre-restoration for better durability and natural occlusion.
- Digital Precision Tools: CAD/CAM workflows simulate insertion trajectories, with 3D-printed prep guides directing burs for parallel reductions—slashing errors by 40% and enhancing enamel preservation.
- Hybrid Implant Integration: For extrema, implants as auxiliary abutments recalibrate paths, blending biologic and mechanical strengths.
The Essential Role of Fixed Orthodontics Mechanics in Modern Practice
In today’s interdisciplinary landscape, proficiency in fixed orthodontics mechanics has become indispensable for prosthodontists, enabling comprehensive care that addresses crowding, diastemas, and abutment parallelism before bridges or crowns. This knowledge fosters collaborative treatment planning, optimizes prosthetic outcomes, and minimizes complications like TMD, while digital tools amplify predictability. Without it, clinicians risk suboptimal restorations; with it, they deliver holistic, patient-tailored solutions.
Patient-Centric Communication in a Global Context
Explaining these nuances—parallelism’s role in averting TMD, the rationale for intrusion, RCT, digital tools, or orthodontic alignment—fosters trust. In multicultural settings, cultural sensitivities around endodontics, surgery, or aligners underscore tailored dialogues, ensuring adherence and satisfaction.
Bridges’ Persistent Global Footprint
Amid implants’ ascent, bridges retain relevance for their affordability, expediency, and minimal invasiveness—crucial in resource-limited areas. The global market, valued at $1.11 billion in 2025, is poised for 5.8% annual growth through 2032, fueled by material advances and digital efficiencies.
Conclusion
In closing, unparallel abutments in dental bridges test our prosthodontic acumen, from TMD-linked occlusal perils to restorative ingenuity. Early vigilance, judicious interventions like guided preps, intentional RCT, or orthodontic straightening via Invisalign, and occlusal recalibration preserve function and well-being. As digital dentistry and ortho-prostho integration evolve, they embody dentistry’s ethos: aligning not just teeth, but lives, with clinical wisdom forged in institutions like RCSI.

Author: Dr. Syed Nabeel, BDS, D.Orth, MFD RCS (Ireland), MFDS RCPS (Glasgow), is a clinician-scholar whose career spans over two decades at the intersection of orthodontics, neuromuscular dentistry, and digitally integrated diagnostics. As Clinical Director of Smile Maker Clinics Pvt. Ltd., he has pioneered a philosophy of care rooted in anatomical precision, occlusal neurophysiology, and contemporary AI-enhanced workflows. A Diplomate in Orthodontics from Italy and an alumnus of advanced programs at Various International Universiteis , Dr. Nabeel brings a globally benchmarked clinical acumen to the nuanced management of temporomandibular disorders, esthetic rehabilitation, and algorithm-guided orthodontics.
In 2004, he founded DentistryUnited.com, a visionary platform connecting over 40,000 dental professionals through peer learning and collaborative dialogue. His academic drive led to the launch of Dental Follicle – The E-Journal of Dentistry (ISSN 2230-9489), a peer-reviewed initiative now indexed in EBSCO, fostering interdisciplinary scholarship across clinical domains.
A prolific educator, he has contributed to UGC and national broadcast media as a subject expert and regularly speaks at scientific forums, favoring small-group, discussion-based formats that emphasize clinical realism over theoretical abstraction. His ethos remains steadfast: knowledge, when shared freely, multiplies in value. Dr. Nabeel continues to shape the future of dentistry through research, mentorship, and his enduring commitment to elevating practice standards in India and beyond.